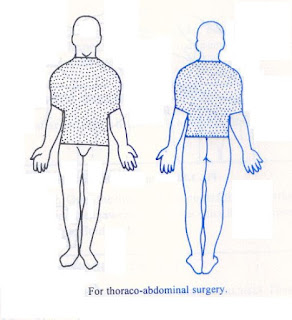
The Operation Site
Shaving
The operation area should be clean before the
operation, and you have to check this in the ward before sending the patient to
the OT (Figs 1.12A to E).
• Shave
the area on the morning of the operation, or as part of operation.
Preparation
Prepare the skin as soon as the patient is
anesthetized.
• Start
with a soap solution, and follow this with spirit
• If
there is a low sensitivity to iodine in the community, use alcoholic iodine
• Take a
sterile swab on a holder start in the middle of the operation site, and work
outwards
• Discard
both swab and holder, and repeat the process with a second swab (some surgeons
use a third)
• The
last is spirit which will evaporate to leave the skin dry
• Be
sure to prepare a wide enough area of skin
• In an
abdominal operation this should extend from the patient’s nipple line to below
his groin.
Draping
The skin has been prepared
• Place
the first towel across the lower part of the operation site
• Place
another towel at right angle on the nearer edge of the operation site
• Apply
a towel clip at the point of crossing of the two towels
• Place
another towel at the far edge of the operation site
• The
final towel goes across the top end of the site. All the corners should have
towel clips to prevent them from slipping, they can go through the skin if the
operation is under GA
• In an
abdominal operation an abdominal sheet covers the abdomen on top of the towels.
This sheet has an opening in its middle to provide access to the operation site
[double toweling]
• If
any area close to the operation site becomes contaminated at any time during
the operation, place another sterile towel over the contaminated site.Any questions be sent to drmmkapur@gmail.com
All older posts are stored i archives for access and review.
Visitors that follow may post contributions to the site.
To create consumer/provider engagement visit www.surgseminar.blogspot.com
www.drmmkapur.blogspot.com